ARTICLES
HIGHLIGHTS
UPDATES
SPOTLIGHTS
EDUCATION
RETROSPECT
ARTICLES HIGHLIGHTS UPDATES SPOTLIGHTS EDUCATION RETROSPECT
ARTICLES
Dr. Ruhul Abid's Journey in Establishing and Advancing HAEFA
Dr. Ruhul Abid, a professor at Brown University, co-founder and president of HAEFA and a Nobel Peace Prize nominee, discusses his journey into public health, providing aid to some of the world’s most vulnerable people, and what he is planning next for HAEFA.
By Ishaan Rahman
Health and Education for All (HAEFA) is a 501(c)(3) nonprofit organization founded in 2012 to address glaring inequalities in healthcare access in Bangladesh. In our interview, Dr. Ruhul Abid, the president and co-founder of the organization and associate professor at the Brown University Warren Alpert School of Medicine, reflected on his path into public health and his work with HAEFA.
Starting out in Public Healthcare
As a newly registered physician, Dr. Abid started his career working for Duncan Brothers, a British tea company, instead of a traditional hospital setting. Dr. Abid's initial exposure to community health was in offering healthcare screening, ensuring effective vaccination among the tea garden workers - raising its coverage from 5% to 97% - and providing routine healthcare services to the organization's employees.
“We developed antenatal checkup, screening for hypertension and diabetes using the community [health workers] in the tea-producing estates...this was often in remote places for the tea pluckers (workers) and their families,” he explained. Through this, he learned how to manage a team, motivate the staff to deliver optimum services and distribute (often limited) resources. "My experience in public health and medical fields proved invaluable in my ability to address the key questions - what are the primary issues? What resources are at disposal? What gaps are there?” He went on. “[My three years at Duncan Brothers] resonated with me in the later part of my life as well."
Building a Team
After moving to the United States and working as a fellow and then faculty at Harvard Medical School, Dr. Abid started thinking about how to give back to the community in Bangladesh. HAEFA resulted from this, an organization co-founded with his colleague at Harvard Medical School, Dr. Rosemary Duda, to provide free healthcare and education to those who needed it most, ranging from garment workers to refugees.
His initial team included many undergraduate and medical students from Harvard University, MIT and Brown University. “I always had some connection with the students,” Dr. Abid says.
Supporting Bangladeshi Garment Workers
The collapse of the Rana Plaza in Dhaka in 2013, which resulted in the tragic death of over 1,100 garment workers, gave Dr. Abid’s new project a renewed sense of urgency and importance. Around a month after the collapse, Dr. Abid visited Bangladesh to investigate the garment workers’ health and safety needs in a workplace prioritizing labor efficiency over wellbeing. “Healthcare was very much neglected,” he sadly remarked.
This became HAEFA’s first major project. A team, including Dr. Abid himself, his daughter, Dr. Duda, undergraduates and medical students, made the trip to Bangladesh. He also contacted colleagues from Dhaka Medical College, which sent physician interns to help. HAEFA’s vital work with the garment workers included screening for non-communicable diseases such as anemia, hypertension, diabetes and asthma. Alongside local healthcare workers, HAEFA also provided health education on safety and personal hygiene. The initial funding for this project came out-of-pocket from Dr. Abid and Dr. Duda.
Early during the project's initial phase, HAEFA encountered a new obstacle. Paper medical records proved too disorganized to keep track of as more patients showed up for screenings. As a solution, “We developed electronic health records (EHR) which could screen one patient in seven minutes,” Dr. Abid said. These efficient tests included BMI, blood pressure, heart rate, on-site hemoglobin, blood glucose monitoring and more. Recognizing the success of this process, the Bangladeshi government provided funds that allowed HAEFA to screen an additional 6,000 patients. The UK’s Department for International Development (DFID) also supported their work.
In 2019, Dr. Abid and his colleagues published key demographic and health data for almost 2,000 Bangladeshi garment workers in the International Health Journal. The research suggested substantial improvement in health screening services when coupled with the use of an electronic medical record (EMR) system.
Raising Awareness in the U.S.
Short on funds, HAEFA worked tirelessly to raise awareness of its work back in the U.S., fundraising at student organizations, churches, mosques, cultural centers and more. Some committed students at Brown University even sold Valentine's Day flowers to raise funds.
HAEFA entered the Grand Challenges Canada competition in 2017, which was sponsored by the Bill and Melinda Gates Foundation and the Canadian government to address global concerns. Dr. Abid joined, displaying HAEFA’s cutting-edge electronic health record (EHR), named NIROG (well-being in Bangla), and screening programs.
“Out of 900 or so organizations worldwide, there were only 43 that received funding and HAEFA was one of them,” Dr. Abid proudly states. The fund alone allowed for the screening of an additional 12,000 patients and arranging new equipment in Bangladesh. However, the "name and fame" that HAEFA acquired from this competition was even more valuable. Dr. Abid proclaimed, "HAEFA became stronger as an organization and in its endeavor."
Facing the Rohingya Crisis
The influx of Rohingya refugees created a new public health crisis at Bangladesh’s doorstep. Wasting no time, Dr. Abid and his team, including fellow Brown University Professor, Dr. E. Jane Carter, traveled to the Cox’s Bazar district in Bangladesh. After receiving approval from the Bangladeshi government to provide healthcare within the refugee camps, HAEFA encountered a new challenge. The electronic patient records, vital to their success with garment workers, would not be workable due to the lack of electricity and internet within the camps. Dr. Abid worked around this barrier by bringing large batteries charged with solar energy.
On the issue of building trust with a persecuted minority, Dr. Abid’s answer was simple: show them results they can understand. Keeping reliable records of their health screening was key to this. Crucially, though, a medium was needed between the volunteers and the Rohingya. “Another thing we did is to include a Rohingya interpreter beside our doctors…that helped us and helped the doctors explain the results and give medicine,” he elaborated. HAEFA volunteers also attended community meetings with their local leaders and Imams.
Tackling the Pandemic
The pandemic dramatically changed HAEFA’s priorities and how they would continue to operate in Bangladesh. First and foremost, Dr. Abid wanted to ensure the safety of refugees from the contagious coronavirus. HAEFA became the first organization to provide refugees and healthcare providers in the hyperdense camps with free masks and hand sanitizer. Additionally, HAEFA educated local healthcare workers in official training programs on the correct protocol to keep people safe. “The pandemic changed us totally, expanding our horizon,” Dr. Abid says.
HAEFA, in collaboration with the Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MoHFW), Brown University, Project HOPE and USAID/Save the Children, developed and launched an Advanced COVD-19 Clinical Management Certification Course for the physicians of Bangladesh in 2021. More than 6,000 physicians have already been trained and certified (by DGHS, Brown University, Project HOPE and HAEFA) through this interactive online course. Another significant contribution of HAEFA during the pandemic was its successful development and training of a Training of the Trainer (TOT) Mental Health Support and Resilience Course for the health workers in Bangladesh in 2021-2022. This Mental Health TOT was a joint collaboration between HAEFA and Project HOPE and has provided support to more than 7,000 health and other workers during the pandemic.
Looking to the Future
Dr. Abid and HAEFA have ambitious plans for expansion of the organization and communities that will be helped. So far, they have planned to start operations in another district, Noakhali. Furthermore, HAEFA seeks to cooperate with Bangladesh’s government to improve clinical research.
In 2020, Dr. Abid’s work in Bangladesh had earned HAEFA and himself the ultimate recognition: a nomination for the Nobel Peace Prize. Ultimately, what started as a small, self-funded organization has become a leader in Bangladesh's public health initiative. HAEFA’s story not only shines light on the obstacles faced towards achieving healthcare justice but also emphasizes the need to address deep-seeded problems within all global communities.
The Rohingya Crisis: Desperation and Hope in the Face of RATION Cuts
Funding cuts by the World Food Programme have left Rohingya refugees with just $0.27 per day for food, entrenching them deeper into this humanitarian crisis. With severe malnutrition, impaired development and increased mortality rates looming, urgent global action is needed to address the dire situation and secure the physical and mental wellbeing of the world's most persecuted minority.
By Raihana Mehreen
The United Nations (UN) has played a crucial role in providing humanitarian aid to the Rohingya. One of the UN's key organizations, the World Food Programme (WFP), operates globally to offer food support to the disadvantaged. At the beginning of 2023, the Rohingya refugees received a monthly food ration of $12 per person, which barely sufficed in meeting their daily needs and, in March, this amount was reduced to $10 (1). On June 1, due to a funding shortfall of $56 million, the WFP implemented a second round of cuts. Each individual is now allocated $8 per month, equivalent to a mere $0.27 per day (1) - within three months, the meager amount of food that the Rohingya did receive decreased by one-third.
Genocidal attacks caused the mass exodus of the predominantly-Muslim Rohingya to Bangladesh in 2016 and 2017 - close to a million now reside in Cox’s Bazar. Already facing decades of persecution, acute trauma and deprivation, health indicators for this displaced population were poor, even before the cuts in early 2023. 45% of families did not have an appropriate diet; 40% of children experienced stunted growth, and more than 50% suffered from anemia (1). Not only so, 20% of Rohingya children under five were malnourished and, consequently, 12% suffered from severe stunting (2). UN experts have warned that the food aid cuts will particularly impact vulnerable populations, including women, especially those who are pregnant and/or breastfeeding, adolescent girls and children (1). The consequences of the reductions are predictable - malnutrition, impaired child development and an increase in infant mortality (1), greatly diminish the potential of future generations of Rohingya. Further exacerbating their formidable living conditions, Cyclone Mocha had struck western Myanmar in May 2023, causing extensive damage to the shelters of around 40,000 refugees.
Growing desperation among the Rohingya has driven them to undertake perilous sea journeys across the Bay of Bengal and the Andaman Sea, hoping to find a better life and reunite with family in other countries. In 2022, over 3,000 Rohingya attempted this voyage on 39 boats. By the end of the year, approximately 160 individuals were still at sea, while an estimated 350 people had either lost their lives or had gone missing (3). Of the 3,040 individuals who disembarked in 2022, 32% arrived in Myanmar, 25% in Malaysia, 24% in Indonesia, 10% back in Bangladesh, 5% in Thailand and 3% in Sri Lanka (3). Those intercepted in Myanmar were arrested and sentenced for violating the 1949 Registration Act or the 1947 Immigration Act that resulted in, respectively, two or five years of imprisonment (3). The new round of cuts may further sway the Rohingya to make the difficult choice of risking their lives to the dangers of the sea, including sailing on rickety boats and being assailed by traffickers and smugglers (1).
Bangladesh has demonstrated remarkable commitment in supporting the Rohingya population since the early 1990s, and particularly after the significant influx in 2017. The Bangladeshi government, along with international organizations and NGOs, has been actively involved in providing humanitarian assistance to the refugees, including food, clean water, healthcare services, emergency relief supplies and education. The Rohingya were deprived of any systematic health care or immunizations since their citizenship was revoked in 1982. In September 2017, responding swiftly to reports of polio and measles outbreaks in the camps, the Bangladeshi government promptly administered emergency vaccines (4). Despite being the most densely-populated country in the world (excluding city-states and small countries), with 1,141 people per square kilometer, Bangladesh has even allocated land to build camps to accommodate the 1.1 million refugees in Cox's Bazar. Kutupalong and Balukhali, HAEFA’s main provision sites, are among the largest refugee settlements in the world.
The utter magnitude of the Rohingya population and the refugee crisis, however, has put immense pressure on Bangladesh's resources and infrastructure. The nation has one of the highest poverty rates in the world; about 31% of the population live below the national poverty line of about $2 per day (4). Recognizing these limitations, Bangladesh has collaborated with international organizations, including UN agencies such as the International Organization for Migration (IOM) and the United Nations High Commissioner for Refugees (UNHCR), intending to identify sustainable, long-term solutions and engaged in diplomatic efforts to address the root causes of the crisis in the attempt to secure the safe and voluntary repatriation of the refugees and ensure accountability for human rights violations.
In addition to the obvious physical ramifications of starvation, the cuts entail a profound mental toll, exacerbating the marginalized state of the Rohingya community and perpetuating cycles of poverty and despair. Amidst this chaos, however, HAEFA stands as a beacon of hope and resilience. HAEFA has established free medical clinics to serve the Rohingya, and on-site providers have cared for over 275,000 patients since October 2017. The dedicated healthcare teams work tirelessly, facing overwhelming challenges, overflowing clinics and relentless heat. Using a portable, innovative, solar-powered electronic medical record system, NIROG (“wellbeing” in Bangla), HAEFA's healthcare workers record patient information on handheld tablets and provide laminated ID cards for systematic record retrieval. This unique approach allows the organization to cater to a significantly larger number of patients which would not have been possible otherwise. HAEFA is the most trusted name in providing quality primary healthcare to this marginalized population due to their effective use of advanced and unique technology, systematic evaluation and the inclusion of human touch in the care of every single patient (4). HAEFA has also established referral systems for various healthcare needs, such as tuberculosis (TB) diagnosis and treatment, safe delivery for pregnant women and malnutrition treatment. The efficient medical teams also provide the host community with quality healthcare as the refugee camp formations make it difficult for the neighboring residents to access care. As the world's largest humanitarian crisis unfolds, HAEFA's goals become more crucial than ever, and as the crisis continues, HAEFA also collaborates with relevant agencies to ensure patients receive specialized care, recognizing the need to build an effective healthcare system to address the long-term needs of the refugees. The Rohingya, scarred by violence and displacement, depend on such organizations to not only heal their physical wounds but also to experience a glimmer of humanity.
This critical situation demands immediate and urgent action from all stakeholders involved. The UN is responsible for securing funding and reinstating food rations in their entirety. The global community must attempt to reinstate the Rohingya's fundamental human rights and implement repatriation to their homeland. We can only aspire to achieve justice and pave the way for a better, safer future for the Rohingya through collective efforts from the UN, international donors and Bangladesh's governing bodies. Undoubtedly, HAEFA stands in solidarity with the Rohingya community as well as with other groups of underserved people in Bangladesh.
We can only aspire
to achieve justice and pave the way for a better, safer future for the Rohingya through collective efforts…
References
(1) UN News, "UN in Bangladesh announces devastating new round of rations cuts for Rohingya refugees," UN News, 25 June 2023. [Online]. Available: https://news.un.org/en/story/2023/06/1137252.
(2) Jason Patinkin, "Rohingya Refugees Facing Malnutrition," VOA News, 17 May 2018. [Online]. Available: https://www.voanews.com/a/rohingya-refugees-facing-malnutrition/4377429.html.
(3) The UN Refugee Agency, “Protection at Sea in South-East Asia - 2022 in Review,” The UN Refugee Agency, 17 January 2023. [Online]. Available: https://data.unhcr.org/en/documents/details/98170.
(4) E. Jane Carter and Ruhul Abid, “A People Without a Country,” Brown Medicine Magazine, February 2018. [Online]. Available: https://medicine.at.brown.edu/article/a-people-without-country/.
HIGHLIGHTS
Brown University and HAEFA Teams Visit District Hospital and FDMN Camp
On May 7, Dr. Susan Cu-Uvin (Professor of Obstetrics and Gynecology, Brown University), Dr. Ruhul Abid (President/Founder, HAEFA and Associate Professor, Brown University), Mr. Monjur Iqbal (Project Director, HAEFA), Dr. Sharmin Sultana (National Clinical Coordinator, HAEFA) and Ms. Raisa Iftikhar (HR Coordinator/Research Assistant, HAEFA) visited the district hospital in Cox’s Bazar. The team met with the assistant superintendents to discuss potential areas for collaboration and methods to enhance the delivery of healthcare services in the facilities.
Dr. Abid and Mr. Iqbal, accompanied by Mr. Md. Mamunur Rashid (Project Coordinator, HAEFA), then visited Mr. Mizanur Rahman, the Refugee Relief and Repatriation Commissioner (RRRC), who is also the Additional Secretary of the Ministry of Disaster Management and Relief (MoDMR), at his office, where Dr. Abu Toha (Health Coordinator, Office of RRRC) was also present. In the meeting, they discussed the overall condition of HAEFA’s health facility at the FDMN Rohingya Camp in Ukhiya as well as fund facilities.
The HAEFA team also visited the Upazila Health Complexes (UHC) in Ukhiya, Maheshkhali, Chakaria and Pekua to observe Non-Communicable Disease Corners that help rural patients with high blood pressure.
Dr. Cu-Uvin and the HAEFA team, including Mr. Saiful Alam (IT Manager, HAEFA), also visited an FDMN Camp in Cox’s Bazar. The team evaluated the quality of services provided to the Rohingya refugees, observed the facilities and engaged with the staff.
Bangladesh's WHO Representatives Visit FDMN Camp
On May 11, Dr. Aroti Singh, Public Health Response Officer and Dr. Raisul Islam, NCD Officer, from the World Health Organization, visited HAEFA’s health post in Kutupalong (Camp 1W) to assess the response to the services provided to the FDMN population.
UPDATES
Comprehensive Healthcare for the Rohingya/FDMNs
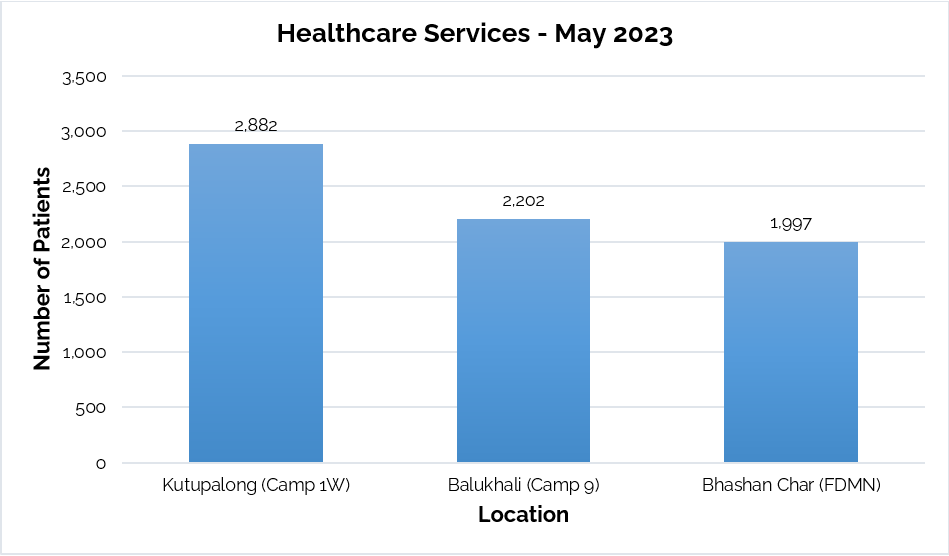
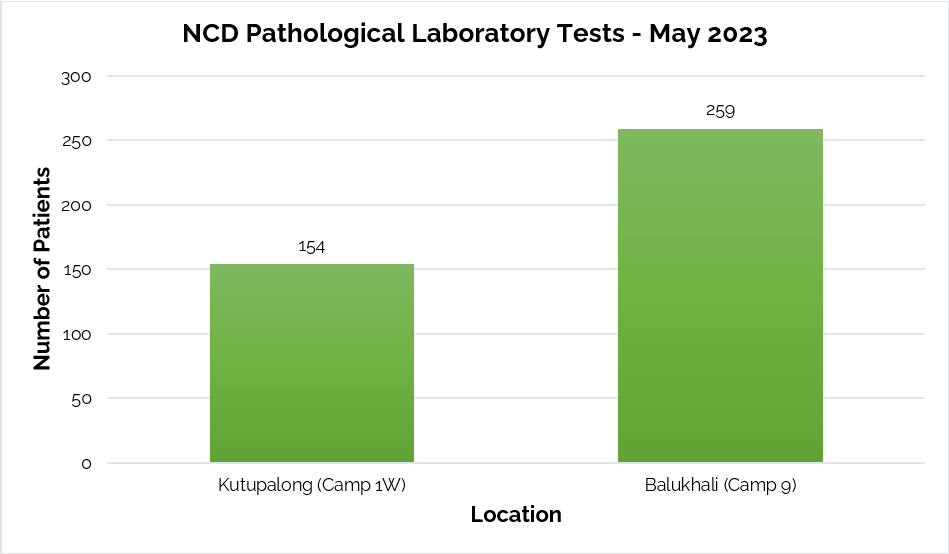
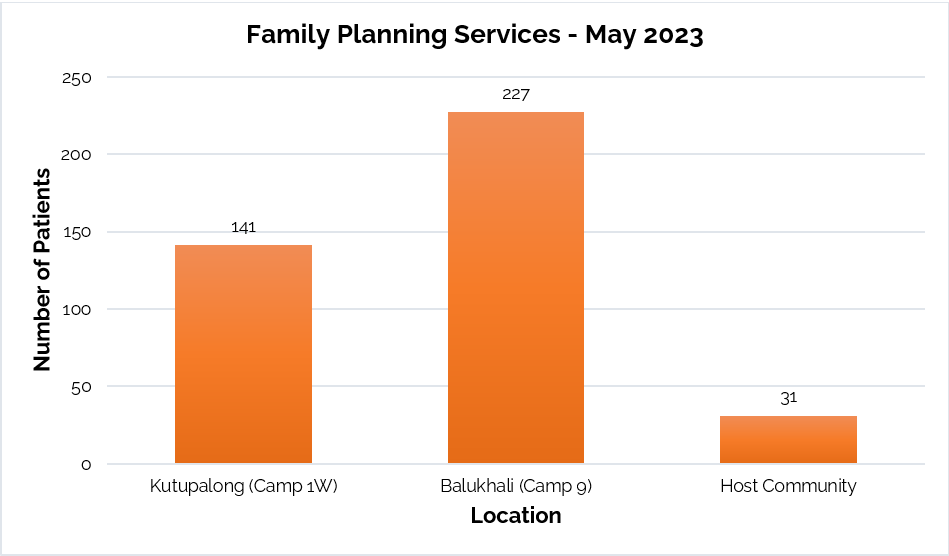
Since establishing refugee camps in Cox's Bazar, HAEFA's healthcare providers have offered free medical care to the Rohingya and Forcibly Displaced Myanmar Nationals (FDMNs). HAEFA has significantly expanded its services over the past six years, focusing especially on providing medical attention in Kutupalong (Camp 1W), Balukhali (Camp 9) and Bhashan Char (FDMN). On-site healthcare services for acute and chronic health conditions include maternal and preventive care, family planning and breastfeeding, health screenings, nutrition education, hygiene and feminine health, immunization programs for children and adults and medication distribution. Blood tests to assess the quantity of red blood cells, white blood cells and platelets (CBC with ESR), urine tests to check for abnormalities of the urinary system (Urine R/M/E) and lipid profile testing to measure blood cholesterol levels are just a few of the many tests performed in the NCD Pathological Laboratories.
MAY 2023
Kutupalong (Camp 1W)
2,882 patients received healthcare services.
154 lab tests were performed by the semi-automated NCD Pathological Laboratory.
141 patients received family planning services.
Balukhali (Camp 9)
2,202 patients received healthcare services.
259 lab tests were performed by the semi-automated NCD Pathological Laboratory.
227 patients received family planning services.
Bhashan Char (FDMN)
1,997 patients received healthcare services.
Host Community
31 patients received family planning services.
This chart displays the number of patients that received healthcare services by location in May 2023.
This chart displays the number of patients that underwent laboratory tests by location in May 2023.
This chart displays the number of patients that received family planning services by location in May 2023.
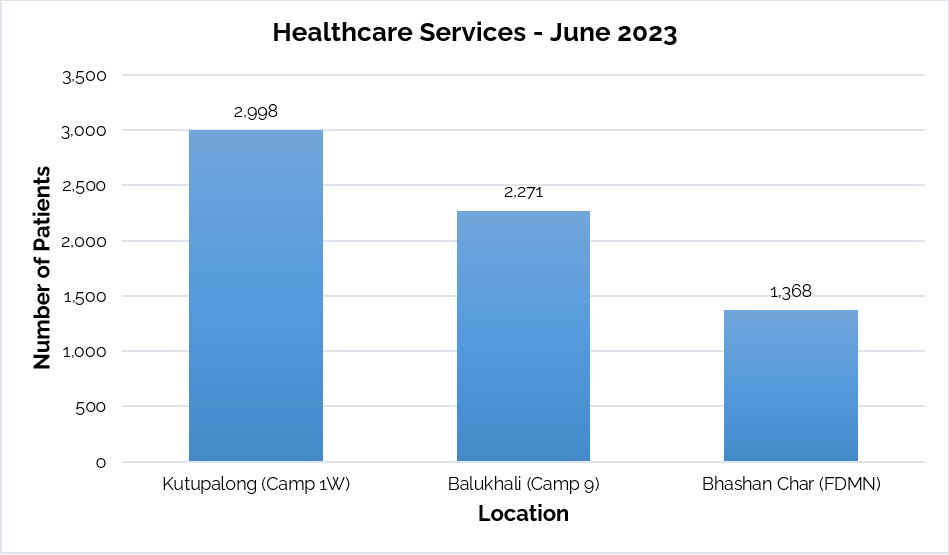
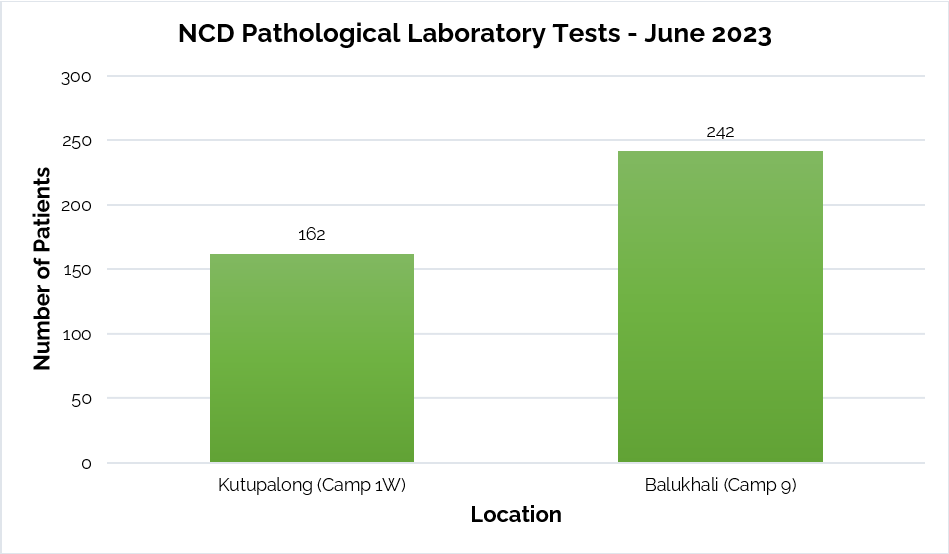
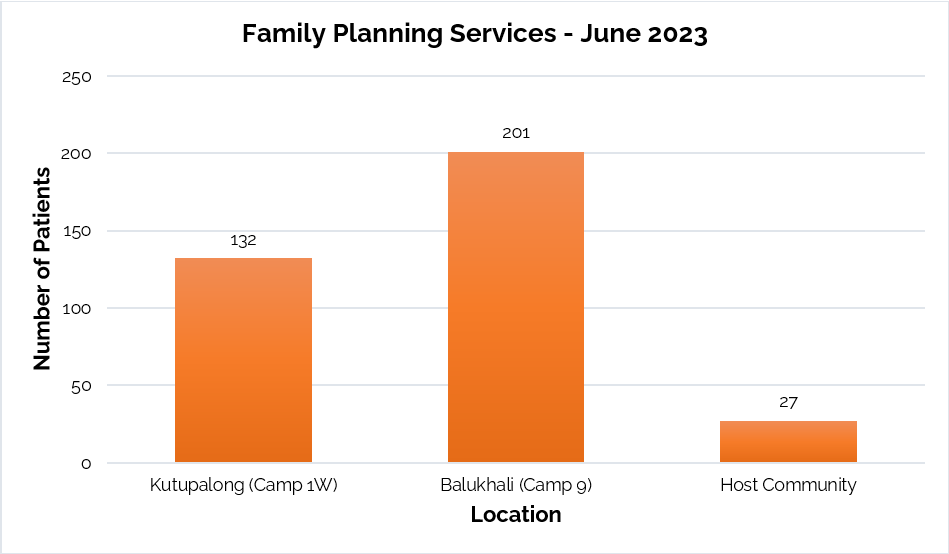
JUNE 2023
Kutupalong (Camp 1W)
2,998 patients received healthcare services.
162 lab tests were performed by the semi-automated NCD Pathological Laboratory.
132 patients received family planning services.
Balukhali (Camp 09)
2,271 patients received healthcare services.
242 lab tests were performed by the semi-automated NCD Pathological Laboratory.
201 patients received family planning services.
Bhashan Char (FDMN)
1,368 patients received healthcare services.
Host Community
27 patients received family planning services.
This chart displays the number of patients that received healthcare services by location in June 2023.
This chart displays the number of patients that underwent laboratory tests by location in June 2023.
This chart displays the number of patients that received family planning services by location in June 2023.
Cervical Cancer Screening Project
There were 5,100 cervical cancer deaths in Bangladesh in 2019, approximately 6.33 deaths per 100,000 women per year. Early detection greatly improves the chances of successful treatment of pre-cancers and cancer and regular screenings prevent cervical cancers and save lives. Cervical cancer is the second most common type of cancer in females in Bangladesh. Apart from regular screenings, which include only screenings and, if needed, referrals, HAEFA also conducts an innovative single-visit See-and-Treat Program to diagnose and treat cervical cancer in its early stages by means of Visual Inspection with Acetic Acid (VIA). This method involves a vaginal speculum exam in which a health care provider applies diluted 3-5% acetic acid (vinegar) to the cervix. A colposcopy is then performed, in which a lighted, magnifying instrument - a colposcope - is used to examine the cervix, vagina and vulva for signs of disease. For those who are VIA-positive, thermocoagulation (using heat to destroy tissue by means of a mobile, reusable, battery-operated handheld device - a thermocoagulator) is a potential treatment. Due to this method, the implementation of NIROG (the electronic health record system for hypertension, diabetes and gestational HTN/DM), HAEFA was awarded the Stars in Global Health by the Grand Challenges Canada in 2018.
Since October 2019, HAEFA has been practicing the See-and-Treat initiative in three sub-districts of Kurigram: Ulipur, Chilmari and Nageshwari. In the past four years, 66,973 have been screened and, among them, 695 were positive. As of 2022, the program has expanded to all nine Upazila Health Complexes (UHCs) and six camps in Kurigram. Recently, HAEFA expanded the screening program to Cox’s Bazar - currently, HAEFA screens women in seven VIA centers (Sadar Hospital, MCWC, Ramu UHC, Moheshkhali UHC, Chakaria UHC, Pekua UHC and Kutubdia UHC) and 11 VIA camps. HAEFA hopes to bridge the gap in diagnosis and care for the many Bangladeshi women at risk of and suffering from cervical cancer through this initiative.
MAY 2023
402 women received regular screenings in Kurigram UHCs - one was VIA-positive, and referred for further investigation and treatment.
966+ women underwent the See-and-Treat Approach in Ulipur, Chilmari and Nageshwari UHCs - seven were VIA-positive, two received thermocoagulation and six underwent biopsies.
1,447 women received screenings at Cox’s Bazar’s VIA centers. 36 were VIA-positive, and referred for further investigation. The CC CXB team, led by Dr. Susan Cu-Uvin (Professor of Obstetrics and Gynecology, Brown University), organized hands-on screenings for VIA-positive patients, from May 7-11; 55 colposcopies and five thermocoagulations were performed at Cox’s Bazar Sadar Hospital, Pekua and Chakaria UHC.
JUNE 2023
360 women received regular screenings in Kurigram UHCs - one was VIA-positive, and referred for further investigation and treatment.
930 women underwent the See-and-Treat Approach in Ulipur, Chilmari and Nageshwari UHCs - 16 were VIA-positive, 16 colposcopies were performed and 11 underwent biopsies.
1,257 women received screenings at Cox’s Bazar’s VIA centers. 12 were VIA-positive, and referred for further investigation. Four colposcopies were performed at Cox’s Bazar Sadar Hospital. The Cox’s Bazar team also followed up with previously-identified cancer patients and referred them to Chattogram Medical College and the National Institute of Cancer Research & Hospital (NICRH), in Dhaka, for further treatment.
Mobile Health Clinics for Host Communities
As the FDMN camp is enclosed with wire fencing, the surrounding host communities have limited access to health clinics, which provide free medical screenings, treatment and follow-ups, in Kutupalong and Balukhali. To help these neighboring residents access care, HAEFA has initiated a weekly Mobile Health Clinic, comprising a Medical Officer, Medical Assistant, Lab Technologist, Midwife and Dispenser. More than 40 patients were treated on opening day in June 2022. Free services include screening and treatment for non-communicable chronic diseases (NCDS), like hypertension, diabetes, asthma and malnutrition, communicable diseases and family planning services. This program aims to improve the quality of life and engender hope for disadvantaged, vulnerable populations.
MAY 2023
174+ host community members received healthcare services at AKNC High School, on the 22nd, and Phalong Model High School, on the 31st, in Ukhiya.
JUNE 2023
141 host community members received healthcare services at Sonarpara High School, on the 12th, and AKNC High School, on the 15th, in Ukhiya.
SPOTLIGHTS
Meet HAEFA's New Editorial Staff!
Raihana Mehreen is the Editor-in-Chief, and joined HAEFA in 2019. She lives in Massachusetts, USA, graduated from Boston University with a degree in neuroscience and public health and is working at WellSense Health Plan.
Sajia Haque is an Associate Editor, as well as the Intern Coordinator for HAEFA, and joined in 2021. She lives in Dhaka, Bangladesh and is a fifth-year medical student at Holy Family Red Crescent Medical College.
Ishan Abdullah is an Associate Editor, and joined HAEFA in 2019. Based in Washington, DC, USA, he is a first-year medical student at the George Washington University School of Medicine and Health Sciences.
Areeb Uzzaman is an Article and Interview Contributor, and joined HAEFA in 2020. He lives in Maryland, USA, and is pursuing an undergraduate degree in international business at the University of Maryland, College Park.
From left to right: Raihana Mehreen, Sajia Haque, Ishan Abdullah and Areeb Uzzaman.
Meet Md. Saiful Alam Sarker, IT Manager!
Evolving over 12 years, Mr. Md. Saiful Alam’s career - which started at a multinational company in Dhaka - culminated in his current role at HAEFA, which began in October 2021, as the IT Manager for the Cervical Cancer Screening Project in Cox's Bazar. His impact has been instrumental in developing the organization's information technology infrastructure, benefiting medical teams that have cared for over 275,000 Rohingya refugees since 2017. “Prior to joining HAEFA, I held the position of System Administrator at various private organizations. I underwent training, gradually building my expertise and advancing in the IT field through diligent efforts, continuous learning and practical experience,” Mr. Alam elaborates.
Mr. Alam was born and raised in Cumilla. His father, now retired, was a manager at Grameen Bank and his mother is a government service holder. Several years ago, when his father fell ill, the family needed to make important decisions regarding treatment. The elder of two brothers, Mr. Alam felt responsible for taking care of his parents, especially because his family always relied on him to make critical decisions, so he aimed to do well professionally. After acquiring an MBA from the University of South Asia (UNISA) in Dhaka and accumulating a decade of IT experience, Mr. Alam is adept at system design and productivity enhancement. He has gained extensive experience in various programming languages and web technologies and has completed CCNA and Windows Server Administration courses, and his toolbelt facilitated notable achievements at HAEFA, including the transition to cloud computing and training initiatives. He relays, “Overall, my passion for technology, the transformative impact of IT in various domains and the guidance from mentors have all shaped my interest and pursuit of a career in IT.” Mr. Alam's passion for the field and its societal impact align with his goals at HAEFA, where he aims to establish a robust IT department. He is currently involved in the upcoming NIROG Plus project, and is aiming for nationwide implementation. Beyond his professional life, Mr. Alam is a family man - a loving husband and father of three who cherishes quality time with loved ones - and enjoys intellectual pursuits, such as reading and staying up-to-date with technological advancements, and sports, especially cricket and football, and watching movies.
Mr. Alam’s IT journey showcases his belief in technology's transformative potential. His hands-on work ethic, communication and reliability underscore his commitment to HAEFA, demonstrating a blend of dedication, ambition and technological prowess. Characterized by a passion for leveraging the field to yield positive societal change, Mr. Alam views technology as a revolutionary force that can elevate health and educational outcomes for underprivileged communities - naturally, Mr. Alam is an invaluable asset. “Since joining HAEFA, my experience in humanitarian work has been truly eye-opening. I am grateful for the opportunity to contribute to meaningful initiatives and make a positive impact,” he proudly states.
EDUCATION
A Quick Overview of HAEFA's Services
Since 2012, HAEFA has provided care for 40,000+ ready-made garment factory workers. In 2017, HAEFA expanded its target population and has cared for 275,000+ Rohingya refugees.
HAEFA has provided aid for many causes, including natural disasters, and is involved in several initiatives, such as COVID-19 response, immunization and women's health.
HAEFA encourages education among underserved populations and prioritizes training to ensure that its staff is well-informed about the latest research advancements.


Retrospect
Ignited Tears: Recounts of a Rohingya Camp Fire
Please help us raise awareness about the plights of the Rohingya by liking, commenting on and sharing this video. Your support can make a difference.
This video illustrates some of the challenges faced by Rohingya refugees after a devastating fire blazed through their camp in March 2023. HAEFA members were on the ground to offer medical and logistical aid and document their stories and needs.
STAFF
Raihana Mehreen
Editor-in-Chief
Ishan Abdullah and Sajia Haque
Associate Editors
Areeb Uzzaman
Article and Interview Contributor
CONNECT
HAEFA has offered free healthcare services to disadvantaged populations in Bangladesh, including RMG workers and Rohingya refugees, and is actively engaged in various initiatives like COVID-19 response, immunization programs and maternal care.
Do you want to help as well?
You are receiving this email because you are subscribed to HAEFA's monthly newsletter.